Oral thrush, also
known oral candidiasis, is a condition that occurs when a fungus called Candida
albicans builds up on the lining of your mouth.
Anyone can develop oral thrush, but babies, young children, older
adults, or anyone with a compromised immune system due to an illness such as
HIV are more susceptible. Conversely, candidiasis lesions can be an early sign
of an HIV infection.
The main symptom of
oral thrush is creamy white lesions in the mouth, usually on the tongue or inner
cheeks. In some cases, the lesions may appear on the roof of the mouth or on
the back of the throat. Thrush is caused when the naturally occurring fungi in
the body get out of balance, which is why the very old, very young, and people
with weak immune systems are at higher risk. Good oral hygiene is an essential
part of treating oral thrush. Healthy adults and children can recover fairly
easily from the infection, especially if they follow a complete oral care
routine of twice-daily tooth brushing and daily proper flossing.
If you are experiencing any symptoms of candidiasis, contact Dr. Brian Williams immediately at (480) 889-1800 for an oral examination.
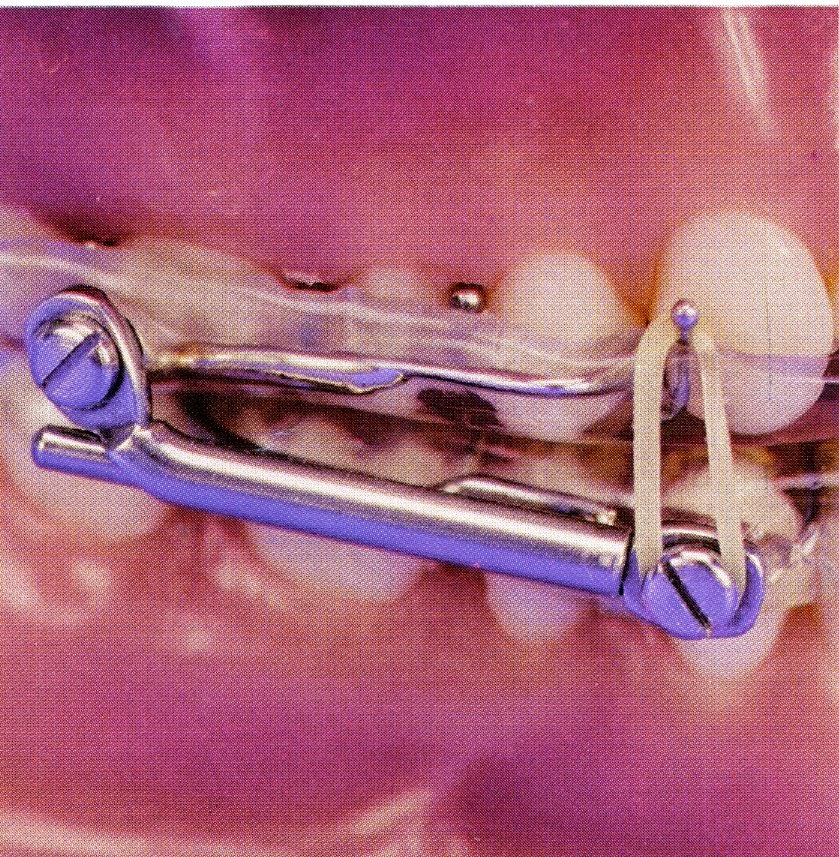
| Peri-implant diseases are inflammatory conditions affecting the soft and hard gum tissues around dental implants. Similar to a natural tooth, bacteria can build up on the base of the implant, below the gum line. Over time, the bacteria irritate the gum tissue, causing it to become inflamed, damaging the tissue and if not caught early, causing the bone structure below the implant to deteriorate. Peri-implant diseases are classified into two categories. | |
In peri-implant mucositis, gum inflammation is found only around the soft tissues of the dental implant, with no signs of bone loss. Generally peri-implant mucositis is a precursor to peri-implantitis. Evidence suggests that peri-implant mucositis may be successfully treated and is reversible if caught early | |
| In peri-implantitis, gum inflammation is found around the soft tissue and there is deterioration in the bone supporting the dental implant. Peri-implantitis usually requires surgical treatment. | Peri-implant mucositis |
| Peri-implantitis | |
Signs of peri-implant diseases are similar to symptoms of gum disease: red or tender gums around the implants, or bleeding when brushing. And just like your natural teeth, implants require regular tooth brushing and flossing and regular check-ups from a dental professional. Other risks factors for developing peri-implant disease include previous periodontal disease diagnosis, poor plaque control, smoking, and diabetes. It is essential to routinely monitor dental implants as part of a comprehensive periodontal evaluation. The up side to dental implants is they function just like your natural tooth. The down side is, they are capable of becoming diseased just like a natural tooth. With a proper oral health routine, your dental implant can last a lifetime. perio.org | |